Healing and coping with irritated eyes is challenging. The eyes are so delicate and sensitive to start. Then, when something irritates the skin around the eyes, a cascade of events can lead to a stubborn rash and persistent state of eye irritation.
I recently experienced a long bout of eye irritation that lasted about a month and is still lingering. It was a small red rash under the lash line of one eye, and some redness on the inner and outer corners of both eyes. For the first week, my skin burned when I put any skincare product around my eyes. It itched at times. I had to stop using all my usual products and suffer from drier skin than usual. It took some time to get my irritated eyes under control.
Coincidentally, someone on one of my social media accounts wrote to me asking for help with the same problem (but much worse in that it had lasted a long time and was making her miserable). That was my ‘sign’ to drop everything and write this post. I suspect a number of you out there may be struggling with irritated eyes too.
WHAT CAUSES IRRITATED EYES?
Irritation can be caused by so many different things. The general term for an irritating rash is dermatitis.
There are different types of dermatitis and the most commonly occurring one is known as irritant contact dermatitis. It is the type most often associated with the use of cosmetic products, and the topic of today’s post. You have probably experienced this at least one point in your life if you used skincare or makeup that didn’t agree with your skin. My eye rash was a classic case of irritant contact dermatitis after using a retinol eye cream that was too strong for me.
This kind of dermatitis is caused by repeated exposure to a particular chemical/substance, heat, or friction.
 An irritant doesn’t have to be a strong chemical. It can be mild. Some common irritants are acids, alkalis, soaps, detergents, and even water. Medications can be irritants too. Did you know some over-the-counter drugs, such as hydrocortisone and the antibiotics bacitracin and neosporin, are sensitizers and cause allergy in some people? So just when you think rubbing hydrocortisone cream on your rash will help, it might actually be making it worse if you have an allergy to it.
An irritant doesn’t have to be a strong chemical. It can be mild. Some common irritants are acids, alkalis, soaps, detergents, and even water. Medications can be irritants too. Did you know some over-the-counter drugs, such as hydrocortisone and the antibiotics bacitracin and neosporin, are sensitizers and cause allergy in some people? So just when you think rubbing hydrocortisone cream on your rash will help, it might actually be making it worse if you have an allergy to it.
When skin is mildly irritated, it can get red, dry, thickened, scaly, and cracked. If it’s fissured (cracked), the skin will sting or burn when it comes into contact with skincare products. Stronger irritants can also cause swelling and ulceration.
Exposure to an irritation doesn’t have to be through physical contact. You can also get irritated by airborne chemicals (e.g. building material particulates such as fiberglass or resins).
An irritating rash can also be caused by heat and repeated friction against the skin, such as a coarse piece of fabric rubbing on skin or repeatedly handling equipment (a common cause of workplace dermatitis).
With irritant contact dermatitis, you notice a change within a few hours if the irritation is acute, or it could be days after multiple applications if the irritant is mild.
Another type of dermatitis is allergic contact dermatitis. A classic example of this is poison ivy or poison oak.
This type of irritation is caused by a chemical that you become sensitized to first, and then over time you develop an allergy to that chemical. It usually takes 1-2 days, but it can take several weeks, months, or even years for the allergy to manifest.
Skin is sensitized first (without symptoms). And then the symptoms show later when the skin is later exposed to the same chemical.
Irritated skin caused by an allergy also develops a rash, but a key difference between allergy and irritant contact dermatitis is itch and swelling. Allergic contact dermatitis is more likely to be very itchy.
Common chemicals that cause allergy are fragrances, preservatives, other ingredients in personal care products, dyes, rubber, nickel and other metals, nail polish additives, and medications. The list is much longer than this of course. Many chemicals can be irritants if they’re at a high enough concentration.
If you have suffered from eczema since childhood, you have atopic dermatitis. This is another type of dermatitis that primarily affects infants and children, but some adults have it too. The clue here is when it starts.
Atopic dermatitis typically starts at an early age and is predominantly a childhood condition (goes away for 90% of children). If it persists into adulthood, it is a chronic, relapsing, lifelong condition that comes and goes. Because the cause is not well understood, and there is no cure for it, it’s very frustrating for people who suffer from it.
Having atopic dermatitis (eczema) tends to exacerbate and complicate other types of dermatitis. So if you have eczema and get an irritant reaction, it can lead to greater sensitivity not just in the place where you got irritated, but over a larger area. In other words, you can start off small and end up with a larger problem. The same thing can happen if you have allergic contact dermatitis.
THE CHALLENGE WITH HEALING IRRITATED EYES
So why have I just taken you through several forms of dermatitis? Does it really matter? Yes if you are struggling with chronically irritated eyes!
Have you ever looked at pictures of rashes? They all look similar, no?
Unfortunately, different types of contact dermatitis have similar visual symptoms. Testing options are very limited too. Therefore, it can be quite difficult to differentiate the different types and identify the correct one based on sight alone. Are you someone who has visited several dermatologists for the same problem and not found any solution? Very frustrating right? You’re not alone. This is one reason!
Much of diagnosis is done through a clinical examination of skin history, product usage, and lifestyle, and ruling out possibilities. In other words, it’s not immediately obvious what the cause is. A doctor needs to look for certain clues and go through a process of elimination.
Add to that, medical solutions for treating dermatitis are limited. Dermatologists rely overwhelmingly on topical or oral steroids and antibiotics. If you’re lucky, these medications solve your problem. If you’re not so lucky, they may provide only temporary relief. Long-term use of steroids isn’t good for skin either – it thins it out, and you can develop sensitivity to a particular one.
With a mild irritant, the rash usually goes away on its own eventually (3-4 weeks). But if your irritation doesn’t go away, then you need to consider the possibility that it has become a chronic condition or you may have an allergy to something. In the latter case, you need to go see a doctor who can do patch testing (a panel of common allergens is applied to the back). Patch testing reveals if you have an allergy to a particular chemical.
If you have atopic dermatitis, well, you most likely already know that.
FIRST PRIORITY: FIND THE IRRITANT
Whether you go to a dermatologist or not, the key to recovering from irritated eyes is to figure out what trigger caused it. The only way to fully heal is to remove that irritant from your routine.
This is a very tall order indeed. What makes it even harder is that many skincare products tend to be made of ingredients from similar chemical families. So removing one irritant may not solve the problem if you substitute that product with a similar one.
Ask yourself these questions:
- Did I use any new product in the last few weeks?
- Did I change my location? Move from one city to another? Am I traveling?
- Did the weather change? Did it get windy, cold, hot, dry, or wet?
- Did I get upset? Am I going through a tough time?
- Did I eat anything different from my usual foods?
Affirmative answers to any of these questions is a clue to the trigger.
If you think it’s a skincare product, try to identify that product. This is a difficult task when you use more than one product. But as difficult as it may be, you have to try because if you don’t remove the offending product from your routine, the irritation can become chronic. Repeated exposure to this irritant can lead to chronic dermatitis.
10 TIPS FOR MANAGING IRRITATED EYES
An eye rash can take a long time to heal completely. Unfortunately, the irritation can be relapsing too. If the nature of your irritation is a chronic condition, you will have to be patient and exercise caution and willpower (the will to avoid experimenting with too many different products out of desperation).
Below are tips that I have found helpful for managing irritated eyes and speeding up the recovery process. They alleviated my own rash. In a blog post, I can’t solve your problem, but perhaps some of these tips can minimize your discomfort. You don’t have to follow every tip. Not all will help you to the same degree.
IMPORTANT NOTE: These tips assume you have a minor case of irritant contact dermatitis. In other words, you DO NOT have a serious rash requiring medical attention, an eye infection (bacterial, viral or fungal in nature), an eye disease, or a disease that has affected your eyes.
1. Go minimal in your skincare routine.
It’s best to leave the rash alone and avoid using any skincare over it and the surrounding area. This may not be comfortable though if the skin is dry (which is what I address in bullet #3 below).
Choose simple products and shelve the potent treatments and creams. Minimize the number of layers and products. Simplify your entire face routine, not just the eye portion.
It’s a nice break for your skin. Less product is not only easier on your skin, but it’s also easier for you to troubleshoot if something should go wrong. With fewer products on your face, you’re more likely to figure out which one is problematic.
Don’t wear makeup over the affected area. No matter how tempting it may be to wear just a little bit of makeup for a short while, don’t. Makeup ingredients are no different from skincare ingredients – they can irritate too. Makeup is also one less thing to clean at night. Makeup stuck or lodged into dry, cracked skin is tougher to remove.
2. Remove all exfoliating products from your routine.
No exfoliating products of any kind, including: exfoliating cleansers & toners, exfoliating/peel pads, exfoliating serums, classic rinse-off exfoliants & scrubs, exfoliating or deep-cleansing masks (deep-cleansing is often exfoliating).
Don’t exfoliate or mask other parts of your face during the time your eyes are irritated. While you may think that it’s possible to avoid contact with the eyes if you’re really careful, the reality is that a tiny bit of product can accidentally get into the eye area, either during application or rinsing.
Exfoliating ingredients are irritating to the eyes even when you don’t have irritation. So, don’t risk aggravating your eyes. It’ll just delay the healing time.
One exception is if you’re treating a small, localized area on the lower face – for example chin and jawline – and you really need to treat it. Stay below nose level then.
3. If you apply a product around irritated eyes – don’t do it to damp or just-cleansed skin.
SCENARIO: Although there is a rash, the skin around your eyes does NOT itch, sting, or burn if you put a product on it. The skin is very dry, tight, and uncomfortable without any moisturizer over it. So you want to put a little bit of cream on it to minimize the dryness.
After cleansing your skin, allow the skin around the eyes to FULLY DRY before you apply any product to the skin.
Now normally, this is the opposite of what you want to do (which is to apply products while skin is still moist for better ingredient penetration).
When your skin is irritated, however, you should delay and slow down ingredient penetration. Moist skin will accelerate ingredient penetration. Absorption takes longer if your skin is dry.
The rate of penetration matters because the skin around the eyes is much thinner than anywhere else on the face and body. It’s why eye skin dries out quickly and wrinkles easily.
When skin is thin or compromised (the barrier is broken), ingredients travel more quickly through the different layers of skin. You have nerves deep inside your skin (the dermis layer) that enable you to feel sensation – for example, heat, cold, and pressure. Those nerve endings will pick up a negative signal sooner when the barrier is impaired. You’ll feel an uncomfortable sensation (burning, stinging, tingling, pain) sooner and more amplified than if your skin were healthy.
When skin is already irritated, ingredients that ordinarily wouldn’t irritate your skin CAN IRRITATE. You may find that a product that posed no problems before now bothers your skin.
So back to my first point – if you’re in the position where you can apply something around the eye, don’t apply it until the skin is dry. You’ll reduce the chance of irritating it.
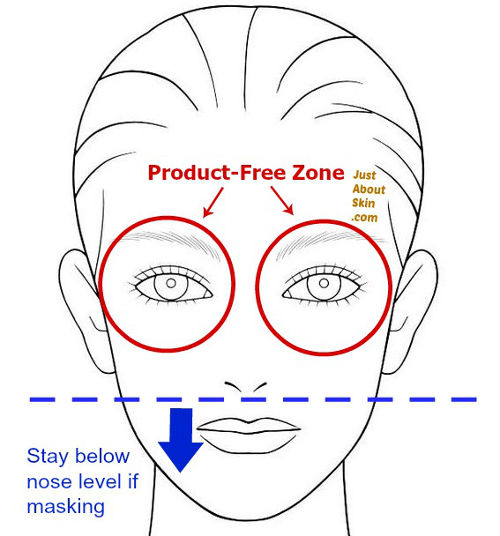
4. If you decide NOT to apply any product around irritated eyes – leave at least a 0.5 inch (1 cm) radius around your eyes free of product.
SCENARIO: The skin around your eyes is reactive. It itches, stings, or burns if you put anything on it. The rest of your face is dry and needs some moisture. So you would rather not leave your whole face completely naked.
Imagine you’re a panda bear. Keep out of the black part of the panda’s eyes.
- stay above the eyebrows
- don’t apply anything on the temples (the side area between the outer eye and hairline)
- stay 0.5-1 inch (1-2 cm) below your bottom eyelash line.
A skincare product can easily ‘travel.’ It doesn’t just go into skin. Directionally, it can spread outward from where you apply it. This spreading action is enhanced when there is already another product on the skin.
For example, if you have just applied oil to your skin, and then you apply a moisturizing cream right afterward, the cream will spread a little. Vice versa too (cream first, oil second – same thing happens).
Ordinarily, this natural migration is quite handy. It makes applying skincare much easier. Any assistance in spreading makes application faster and more economical (you end up using less product).
But in the case of irritated skin, you don’t want any of your facial products accidentally migrating into the eye zone.
For example, cream applied to the cheekbones can seep into the lower eye area. If that cream is designed to treat a problem such as aging or acne, it has ingredients that are active and stimulating. Those ingredients can irritate the eyes.
5. Work on other parts of your face first and save the eye area for last.
This will allow more time for the skin around the eyes to dry. For example, you could apply your products to one cheek, then the next cheek, then the nose, then the forehead, then the neck. And finally, the eyes (if you are going to put something there).
Try to wait at least 5 minutes before you work on the eyes. If you can’t wait that long, come back later when you do have some time. It’s ok to allow hours to pass when you’re in this situation.
When my eyes are irritated, my normal concern about eye skin getting dried out goes out the window. I don’t worry about that. My primary objective is getting the skin to heal ASAP because allowing it to stay in a chronically irritated state will do more damage to my skin long-term than leaving it dry. Dry skin can be brought back to normal moisture levels later.
6. If you’re layering multiple skincare products on the rest of your face, allow a product to FULLY DRY before you add another layer of product.
This goes back to bullets #3 and #4 – a skincare product that’s already applied to skin will enhance penetration or spreading of the next product.
If you don’t give your skin enough time to absorb a layer, it will spread more laterally than it will penetrate into skin. Spreading is what you want to avoid, because spreading can allow product to seep into the eye zone.
7. Watch out for weak spots on irritated eyes when applying skincare.
 What I call the weak spots for the eyes are the outer corners and inner corners.
What I call the weak spots for the eyes are the outer corners and inner corners.
The outer corners can fissure easily (crack, exposed and red). Ingredients will sting if they pass through a fissure in skin (it’s like an open wound).
The inner corners are more sensitive too. Ingredients can irritate the inner tissue (the part that’s pink and connected to the eyeball) if they enter through the inner corner.
Avoid applying products directly over or near these weak spots if you decide to lightly moisturize the eye area.
8. Don’t apply eye masks, eye gels, eye pads, or sheet masks that are designed to soothe tired eyes.
In spite of their intended purpose, the ingredients in those eye masks or pads will likely do the opposite of soothing if your skin is already irritated (for all the reasons I’ve already stated).
Save those products for when your skin is back to normal.
9. Use a cleanser only once a day – at night.
Keep irritated skin unperturbed as much as possible. This means keeping products to a minimum – not just lotions and creams, but cleansers too. When skin is irritated, you should minimize going from dry-to-wet.
 Use cleanser at night when your skin is dirtier after a full day of exposure to its environment.
Use cleanser at night when your skin is dirtier after a full day of exposure to its environment.
In the morning, rinse your face with lukewarm water, unless you are very oily and have serious acne (in which case you should cleanse gently with a mild cleanser and keep that away from the eyes).
Don’t put cleanser directly on the affected area if it’s very irritated. Even lightly touching an irritated area can inflame it further.
The exception is if you need to remove mineral sunscreen or makeup that has seeped into the eye area. So long as the irritation isn’t serious, you can cleanse it with a gentle cleanser.
10. Don’t rub or scratch irritated eyes.
Rubbing or scratching an itch feels good temporarily. But you should resist the temptation. Rubbing antagonizes an area that’s already inflamed. Scratching makes skin thicker, which will itch even more. And then you end up in vicious scratch cycle.
If you’re very itchy, you can consider taking an over-the-counter antihistamine (for allergy relief), but check with your physician first.
WHEN TO SEEK MEDICAL CARE
For irritated eyes, it’s tough knowing when you should call up the doctor. You may be wondering – will my rash go away on its own or is it more serious? These days, at least in the U.S., it’s hard getting an appointment with a dermatologist right away (using insurance). So you may be wondering at what point should you be seeking professional help and making that appointment.
Unfortunately, I can’t give you that answer. Only a medical professional can advise you. My basic rule of thumb is to err on the side of caution. Whenever in doubt, play it safe and seek medical help, even if it’s inconvenient or difficult to schedule an appointment. There are many reasons why you may be experiencing irritated eyes, and they share similar visual signs. Only a physician can assess the problem through a clinical examination.
Here are some signs that you may need to see a doctor if you have irritated eyes. It is not an exhaustive list. Just some examples.
- a large and rapidly growing bump (that’s not a pimple)
- a cluster of bumps that’s spreading rapidly (that’s not acne)
- pus oozing from your skin or skin that is ‘weeping,’ with pain
- open exposed skin, popped blisters
- a scaly discolored rash that won’t go away
- a “growth” that is getting larger rapidly (this could be skin cancer)
- pain, fever, chills (these are typical signs of infection)
- cloudy vision, changes in your vision
- very red eyeballs (the white part) or extremely itchy eyes
Basically, anything changing or spreading rapidly should get examined. If it looks bad or scary to you, assume it’s not good and get a doctor to confirm for you. Don’t hope it will go away and wait some more. Your eyes are essential organs to say the least. Unlike a rash on your arm, for example, you don’t want to take any risks with the eyes.
Stay tuned – my next post will continue this topic on irritated eyes and focus on products to use.
Want new articles delivered straight to your inbox? Sign up here.
Related Reading: